Listen to the article
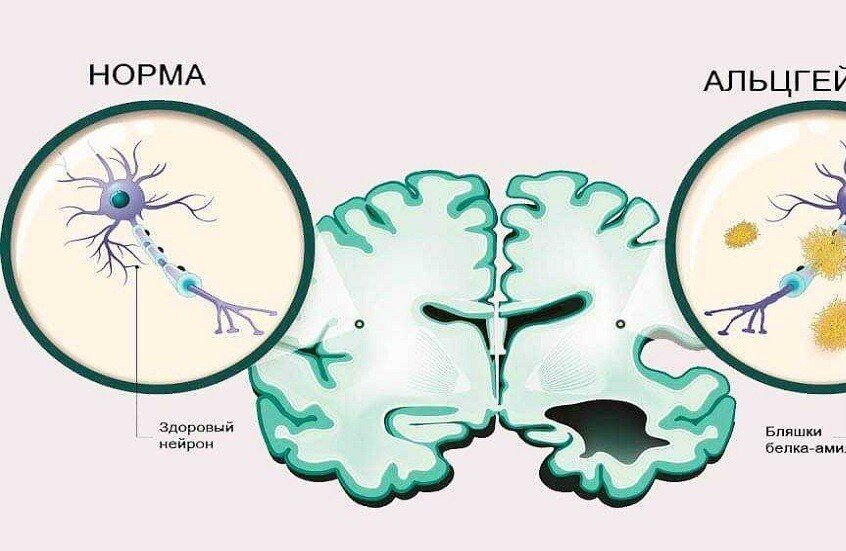
A recent American study has revealed that excessive protein accumulation in brain blood vessel walls significantly increases dementia risk in older adults. According to the research, this condition known as cerebral amyloid angiopathy raises the likelihood of developing dementia by approximately four times within the following five years, highlighting a critical connection between vascular health and cognitive decline.
The study was conducted by researchers at Weill Cornell Medicine, led by Assistant Professor Samuel Bruce. The team analyzed medical records of 1.9 million older adults in the United States who sought hospital care between 2016 and 2022, comparing dementia rates among those with and without the vascular condition.
Understanding Cerebral Amyloid Angiopathy and Dementia Risk
Cerebral amyloid angiopathy represents a common vascular disorder affecting elderly populations. According to Bruce, the condition involves the accumulation of protein waste within the walls of small capillaries and medium-sized arteries in the brain. This buildup makes blood vessels vulnerable to damage and increases susceptibility to strokes, brain hemorrhages, and other forms of internal brain injury.
However, previous research had not comprehensively evaluated how frequently and how rapidly cognitive problems develop in patients with this condition. The current study aimed to fill this knowledge gap by focusing specifically on how protein accumulation itself affects dementia risk and cognitive disturbances in affected individuals.
Significant Findings on Protein Buildup in Brain Vessels
The research findings revealed striking differences in dementia rates between patient groups. According to the study results, 42 percent of older adults diagnosed with cerebral amyloid angiopathy developed dementia within five years. In contrast, only 10 percent of other patients without the condition received a dementia diagnosis during the same timeframe.
Additionally, the study examined how stroke events influenced outcomes. Researchers found that dementia risk increased 4.5 times among patients with cerebral amyloid angiopathy who also experienced a stroke. Meanwhile, patients who suffered brain hemorrhage without the underlying vascular condition showed a 2.4-fold increase in dementia risk.
Vascular Disorder as Independent Risk Factor
One particularly noteworthy finding involved comparing patients with the vascular disorder across different clinical presentations. Bruce noted that researchers observed no substantial differences in dementia risk among patients with cerebral amyloid angiopathy, regardless of whether they had experienced a stroke. In both scenarios, the risk remained significantly higher compared to other patients who suffered brain hemorrhage without the protein accumulation disorder.
This pattern suggests that the vascular disturbance itself contributes to dementia development independent of acute events. The protein buildup in brain blood vessel walls appears to create conditions that promote cognitive decline through mechanisms that extend beyond stroke-related damage alone.
Implications for Dementia Prevention Research
The study’s conclusions emphasize the need for further investigation into underlying biological mechanisms. According to Bruce, while the research establishes a clear association between cerebral amyloid angiopathy and accelerated cognitive decline, the precise pathways through which this occurs require broader investigation. Understanding these mechanisms could potentially open new avenues for therapeutic intervention.
Furthermore, the findings underscore the importance of vascular health in maintaining cognitive function during aging. The research adds to growing evidence that brain blood vessel integrity plays a crucial role in preventing dementia, suggesting that monitoring and addressing vascular conditions may represent an important preventive strategy.
Researchers indicate that additional studies will be necessary to determine optimal screening protocols and potential treatment approaches for elderly patients with protein accumulation in brain vessels. The timing and methods for identifying at-risk individuals remain subjects requiring further clinical investigation.