Listen to the article
Hidden fat accumulation in internal organs is linked to accelerated brain aging and cognitive decline, even in individuals who do not show outward signs of obesity, according to new research. Scientists from the Hospital of Suzhou Medical University have found that the location of fat deposits, rather than overall body weight, plays a crucial role in determining neurological health risks. The findings suggest that visceral fat poses a significant threat to brain health regardless of a person’s external appearance.
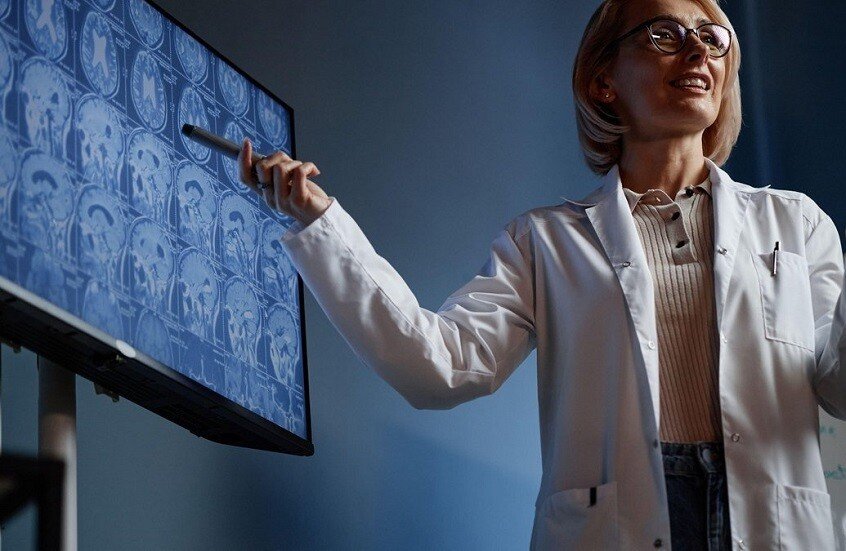
The study, published in the journal Radiology, examined multiple patterns of fat distribution using magnetic resonance imaging (MRI) scans. Researchers identified that hidden or localized fat, meaning adipose tissue accumulating in organs rather than under the skin, produces the most negative changes in brain structure and function.
Hidden Fat Patterns Linked to Brain Deterioration
According to the research team, two specific patterns of fat distribution pose particular risks to neurological health. The first involves elevated fat levels in the pancreas, a condition known as pancreatic steatosis. The second pattern is characterized as “lean but with excess fat,” where individuals maintain normal body weight but have high proportions of adipose tissue internally.
The study revealed that participants with pancreatic fat accumulation had fat percentages around 30 percent. This represents two to three times the percentage found in other participants and up to six times higher than individuals with normal fat distribution patterns.
Impact on Brain Structure and Cognitive Function
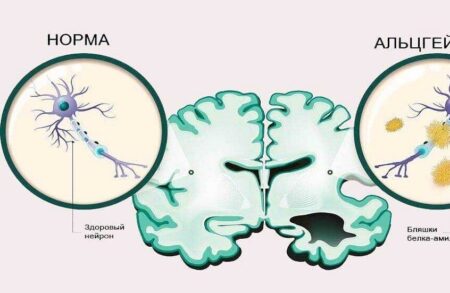
Both problematic fat distribution patterns were associated with reduced gray matter volume and the appearance of white matter lesions in the brain. Additionally, researchers observed decreased cognitive performance, particularly in reaction speed and memory functions. These changes resemble signs of accelerated brain aging and were more pronounced in male participants, according to the study.
The implications extend beyond structural brain changes. Further analysis of medical data demonstrated that these fat patterns correlate with increased risks of neurological disorders. In lean men with excess hidden fat, the risk of depression was nearly three times higher, while stroke risk approached double that of individuals with healthier fat distribution.
Gender Differences in Hidden Fat Health Risks
Women experiencing fat accumulation in the pancreas faced even more concerning risks. The research indicated that these women had more than double the risk of stroke compared to those with normal fat distribution. Furthermore, their risk of developing epilepsy was more than three times higher, highlighting significant gender-specific vulnerabilities to visceral fat accumulation.
The findings challenge conventional understanding of obesity and metabolic health. Many individuals who appear healthy based on standard weight measurements may actually carry dangerous levels of visceral fat. This hidden fat in internal organs can trigger inflammatory processes and metabolic disruptions that accelerate cognitive decline, even when body mass index falls within normal ranges.
Implications for Health Screening and Prevention
These results underscore the limitations of relying solely on external appearance or body weight as indicators of metabolic health. The study suggests that comprehensive health assessments should include evaluation of internal fat distribution patterns, particularly pancreatic fat levels. However, access to advanced imaging techniques like MRI remains limited for routine screening in many healthcare settings.
The connection between visceral fat and brain health also points to potential prevention strategies. Lifestyle modifications targeting internal fat reduction, rather than simply weight loss, may prove more effective in protecting cognitive function. Nevertheless, the specific mechanisms by which hidden fat accelerates brain aging require further investigation to develop targeted interventions.
Further research is expected to explore therapeutic approaches for reducing visceral fat accumulation and determining whether such interventions can reverse or slow cognitive decline. The researchers have not yet announced plans for longitudinal studies to track how changes in fat distribution patterns affect long-term neurological outcomes.